Hemorrhoids, the taboo subject - don’t sit them out!
What are hemorrhoids?
First of all: We all have hemorrhoids. This is the name given to the vascular cushions at the end of the rectum, and are responsible for sealing the anus. This means that they support the sphincter muscles and ensure stool continence. Without them we would not be able to control our bowel movements. This cushion of blood vessels can swell and shrink. When the rectum fills up, this cushion is supplied with a lot of blood and swells. How long does it take for hemorrhoids to subside? Immediately after a bowel movement, this area usually relaxes again, the cushion contracts and carries less blood. So far, so good.
However, if these vascular cushions are permanently enlarged, it indicates hemorrhoidal disease, and the typical symptoms ensue. There may be a secretion leaking from the anus which leads to itching and burning.
Nothing to be ashamed about!
Hemorrhoids are unfortunately still considered taboo. That is why those affected ignore the problem until the symptoms are intolerable. Only 4% of all affected people visit a doctor they trust, the rest are on a secret mission. You think the ostrich tactic is good? But here comes the bad news: it can get worse, you are faced with a series of inconveniences, as this condition is usually a progressive one. Additionally, because the skin is hanging out, it is hard to implement thorough hygiene, which can lead to inflammation. Excessive rubbing or itching of the skin on the anus, which is already irritated, can cause damage and painful anal fissure. This area can become a breeding ground for bacteria and germs, and when this occurs, it‘s no laughing matter.
Very important: Enlarged hemorrhoids are a widespread problem; statistically, almost 70% of adults in industrialized countries are affected at least once in their lives.
Video-Recording
What do hemorrhoids look like?
The appearance of hemorrhoids depends entirely on the severity of the disease.
First degree hemorrhoids
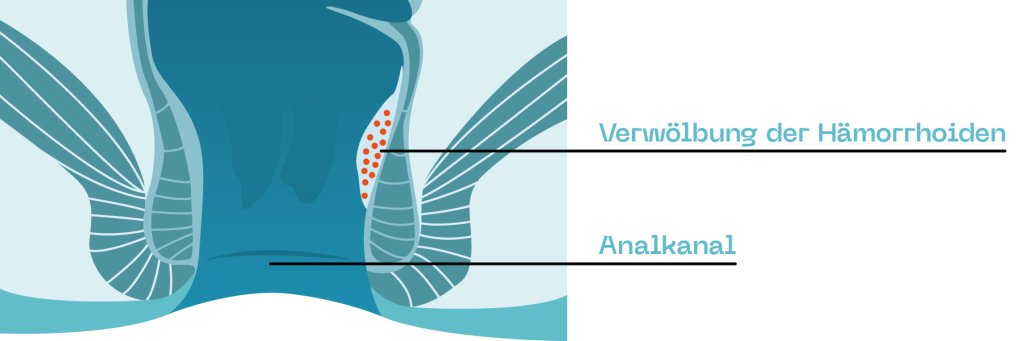
In grade 1, they are only slightly enlarged, and only slight discomfort or perhaps nothing at all has been noticed.
Grade 2 hemorrhoids
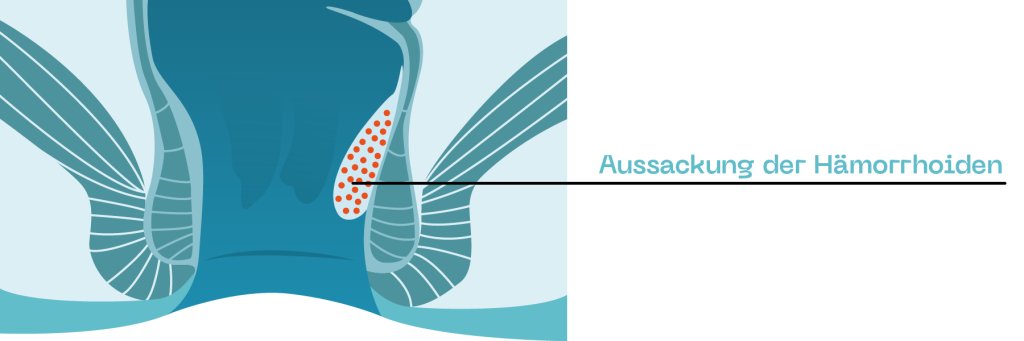
In Grade 2, the hemorrhoids come out during defecation and then retreat afterwards.
Grade 3 hemorrhoids
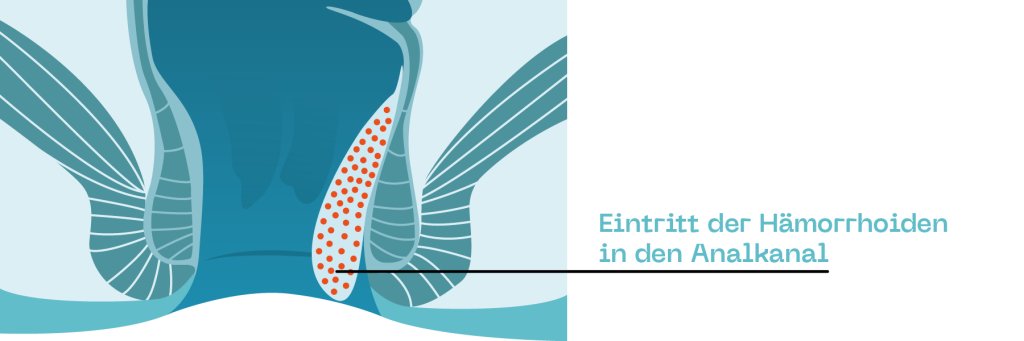
Grade 3 is when the hemorrhoids that have come out after defecation no longer recede on their own and have to be manually pushed back into the anus.
Grade 4 hemorrhoids
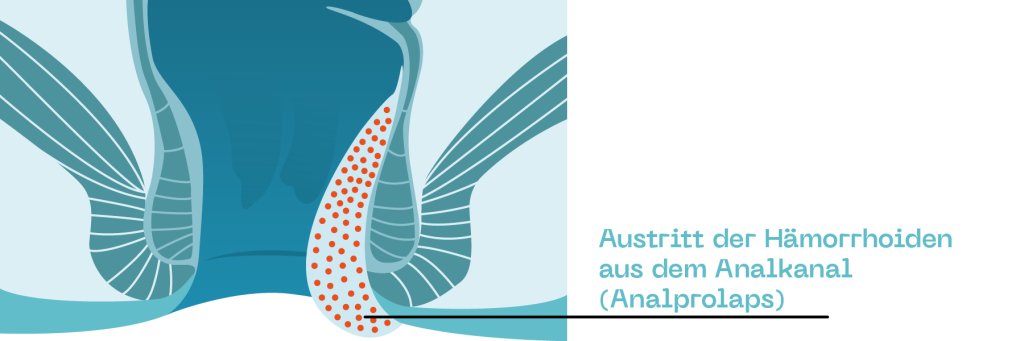
The situation becomes even more uncomfortable in the case of grade 4 hemorrhoids: Here, the hemorrhoids are completely prolapsed and cannot be pushed back into the anal canal. As a result, they become trapped in the anus and swell even more, causing severe pain. At this point, it usually means: Off to the doctor!
Causes of hemorrhoids

How do hemorrhoids develop?
Several risk factors are discussed. Overweight, low-fibre nutrition, lack of exercise or even a congenital or age-related weakness of the connective tissue are blamed for this, but also lifting heavy loads, frequent diarrhoea or laxative abuse.
Pregnancy can also be a possible cause of hemorrhoids. The resulting weight gain and the resulting increase in pressure in the abdominal cavity obstructs the outflow of blood from the erectile tissue. This is why pressing during harder bowel movements or the resulting pressure can cause hemorrhoids, as is the case with chronic constipation, for example.
Did you know that children can also suffer from hemorrhoids? In most cases the reason is constipation.
Hemorrhoids: Symptoms
Blood in the stool
If hemorrhoids show symptoms, these are usually not very specific and hardly differ from those of other proctological diseases. However, one of the most important first signs is blood in the stool or on toilet paper, as hemorrhoids often bleed after defecation. This happens because the increased pressing causes more blood to accumulate in the vessels. Usually, hemorrhoids bleed very little in the early stages, but develop into heavy bleeding in advanced stages of the disease. At this point, a doctor visit would be necessary.
But be careful, the colour of the blood is crucial. Bleeding hemorrhoids give off light red blood; darker blood can be a sign of other intestinal diseases.
Itching – anal itching - Pruritus ani

Itching is also typical for hemorrhoids. But why do hemorrhoids itch? Because hemorrhoids have lost their ability to function, the anus is no longer completely tight and fluids and stool residue leaks into the anal fold. These irritate and damage the surrounding skin long term and an annoying itching (pruritus ani) develops.
Are you suffering from these symptoms? Click here to access the blog post about anal itching.
Further symptoms for hemorrhoidal disorders
A burning sensation in the anus, foreign body sensation, weeping, slimy discharge, sore skin in the anal region, palpable protrusions or a feeling of pressure in the rectum are further symptoms of this unpleasant disease.
Although diarrhoea is not one of the typical complaints, faecal incontinence can occur during the course of the disease because the anus can no longer seal completely.
Pain

A rather untypical symptom of hemorrhoids is pain. This occurs - if at all - only in very advanced hemorrhoids (severity grade 4).
Caution, danger of confusion: If there is stabbing pain in the anal region, a perianal thrombosis may also be the case. This is a pea- to plum-sized, often blue shimmering nodule on the anal edge, which is sometimes also called "external haemorrhoid" and occurs within a very short time. As with real hemorrhoids, they are caused by blood clots, the venous plexus around the anus is affected here. This normally resolves itself on its own, and a surgeon would only operate on large ones.
What to do in case of hemorrhoids - when to consult a doctor?

If you suspect that you are suffering from hemorrhoids, it is best to see a doctor immediately. But which doctor treats hemorrhoids? The specialists for hemorrhoids are undoubtedly internists or gastroenterologists, but even more specialised are proctologists, who deal exclusively with troublesome issues of the rectum. After a thorough anamnesis, in which the doctor also clarifies stool frequency and eating habits, an inspection of the anal region as well as a proctoscopy, i.e. an examination of the rectum, usually follows. In some cases, a colonoscopy may also be indicated in order to rule out other possible causes of bleeding.
What helps against hemorrhoids?
If you want to treat hemorrhoids, there are fortunately different treatment methods, depending on the severity of the condition. For lighter stages, home remedies and local medicines are used or icing or sclerotherapy is considered. Only if all of these measures have been exhausted without signs of improvement are surgical procedures used. Very important: With this disease it is absolutely necessary to always clean the bottom as thoroughly as possible after bowel movements in order to reduce the occurrence of secondary diseases.
Optimized anal hygiene - prevent and alleviate with ProctyClean®
Thorough anal hygiene is incredibly important, especially in the case of haemorrhoidal disorders. Although this does not improve the hemorrhoids themselves, it certainly impedes the development of secondary diseases. These secondary diseases can make life very difficult. As already mentioned, enlarged hemorrhoids prevent a tight seal in the anus, and stool and fluids can get into the outer anal area. The irritating substances contained damage the delicate skin around the anal area and inflammation, itching and even annoying anal eczema can develop. But beware: It is important to avoid scrubbing your backside with aggressive soaps and washing lotions, because the ingredients contained in them can sometimes make the situation go from bad to worse. Moreover, conventional methods can only be used to cleanse the outer anal area.
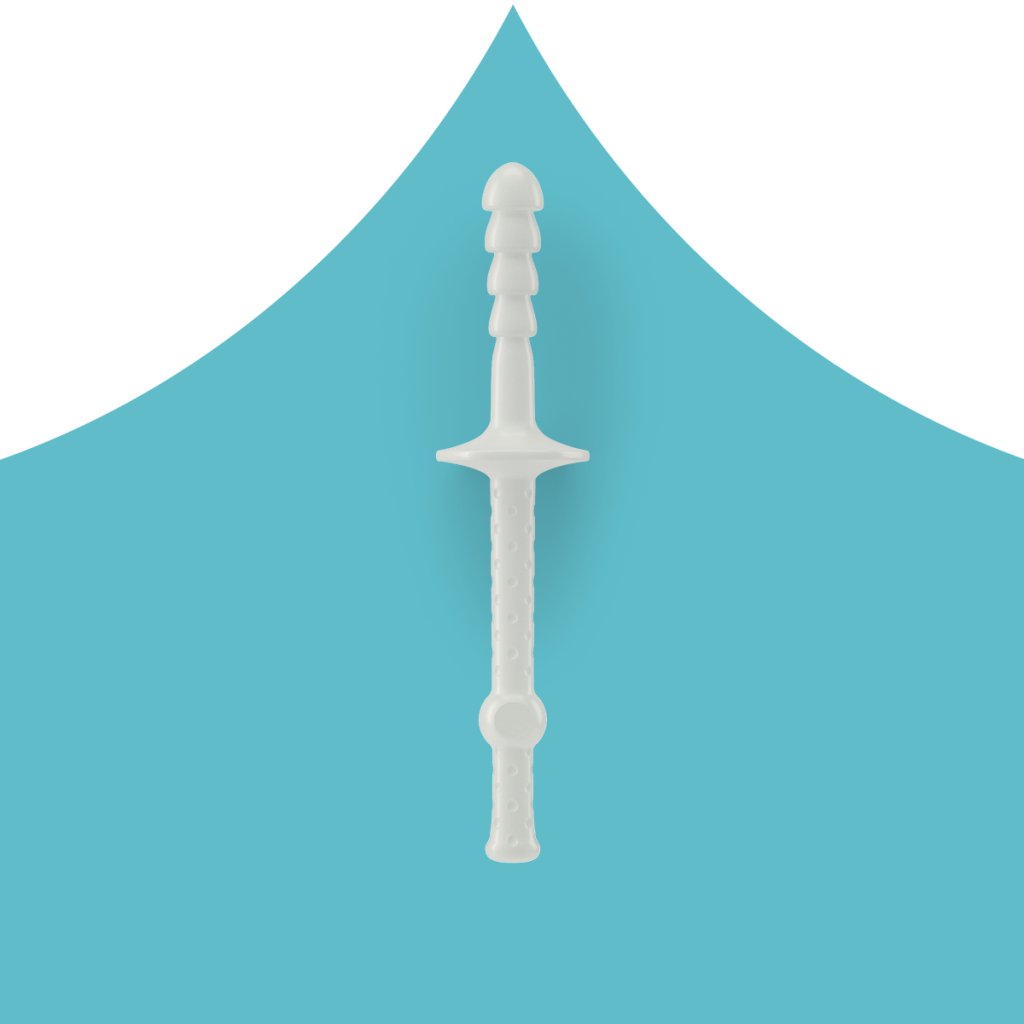
With the patented ProctyClean® intimate hygiene pen, you are able to easily access and cleanse the source of the irritating substances, namely in the anal canal. The application, done after a bowel movement, takes just 1-3 minutes. ProctyClean quickly removes virtually all remaining stool residue from the end of the anal canal and the sensitive anal skin folds. There is no more anal leakage, you feel clean and you stay clean.
Treatment of hemorrhoids with medication: pain go away!
Locally applied medications can be helpful at any stage of the disease - some have an anti-inflammatory effect, others are local anaesthetics. Ointments are simply placed in the anus using an applicator. If you don't want to do this, you can also put the ointment on a compress and then use it as an insert. Some active ingredients work on the spot in the form of a suppository.
Remember, these pharmaceuticals only alleviate symptoms. The possible irritating cause (stool residue, etc.) still lurk in the anal canal. It is important to clean the anal canal before applying any medication. ProctyClean provides the perfect cleaning solution to properly prepare for medication application. After all, you would not want to put a plaster or ointment on a dirty wound!
Hemorrhoid ointment

There are numerous haemorrhoid ointments, pastes and suppositories available in pharmacies to inhibit inflammation and relieve pain. Always check with your doctor before use! Anti-inflammatory active ingredients are zinc, panthenol or also herbal remedies such as witch hazel or aloe vera, which are specialised for skin irritation and itching. Ointments containing cortisone, e.g. prednisolone or hydrocortisone acetate, are also highly effective. These special agents inhibit the immune system and thus counteract the inflammation. But be careful not to use cortisone for too long as this may result in skin atrophy or a fungal infection.
Local anaesthetics
Local anaesthetics have the advantage that they provide targeted pain relief, and the affected person can finally breathe without pain. Unfortunately, however, local anaesthetics such as benzocaine and lidocaine may only be used for a short time, as short and long term use may cause an allergic reaction.
Sclerotherapy, icing or ligation of the hemorrhoids
For grades 1 or 2, various minimally invasive procedures can provide relief. For example sclerotherapy, in which the doctor injects a tissue-shrinking agent into the vascular inflow of the hemorrhoids. The vessels become smaller and retract into the rectum. Although sclerotherapy by means of irradiation with infrared light also exists, this method is considered less successful. The method of freezing (nitrous oxide, liquid nitrogen) is sometimes used, although it remains controversial due to inconsistent success.
Ligation of the hemorrhoids, also called rubber band ligation, is a very successful method used to treat mostly Grade 2 and sometimes Grade 3 cases.
How does it work? The doctor ties off the hemorrhoidal nodes with a rubber band, so that the blood supply can be interrupted and the tissue can die. The hemorrhoid falls off one to two weeks later and is excreted naturally. It might sound scary, but it is very effective and virtually painless!
Hemorrhoids surgery: Rien ne va plus - when nothing else works

The last resort, i.e. when the condition has reached grade 3 or 4, is the surgical removal of hemorrhoids, call a haemorrhoidectomy. This involves individual sections or can be performed in a circular pattern. The tissue can be removed with scissors, scalpel or laser. In some procedures the wound remains open after the operation, in others it is partially or completely closed.
Depending largely on the severity of the problem and a risk-benefit analysis, the doctor will decide which method is best. Dr. Longo developed a method used since 1998, which is considered to be particularly painless. It is the method of choice for grade 3 hemorrhoids. In this procedure, the hemorrhoids are removed with a stapler and the edges of the wound are stapled. Due to a higher risk of relapse, other surgical methods are preferred for Grade 4 hemorrhoids.
Hemorrhoid household remedies
The use of household remedies would only be recommended for Grade 1 and 2 hemorrhoids. However, the following applies here: Please use caution! Some home remedies are touted to be miracle cures, but the results leave much to be desired and may only bring relief for a short time.
Hemorrhoid hip bath

There seems to be an herb grown for every ailment - and this also applies to hemorrhoids. Externally, soothing hip baths with oak bark extract can be used to reduce itching in the outer anal region. Witch hazel, yarrow, horsetail or sweet clover and chamomile have a soothing effect on the skin. Instead of a hip bath, compresses with black tea can also provide relief. It is important to discuss these options with a doctor or pharmacist as essential oils can also be problematic for irritated skin areas.
Hemorrhoids and the importance of nutrition

Correct nutrition is essential for hemorrhoids. After all, a(nal) and o(ral) are more than clearly connected in this case. Therefore, certain foods can also help to alleviate hemorrhoids. It is particularly important to eat a diet rich in fibre to keep the stool soft and supple. Whole grain products, pulses, lots of vegetables and fruit are recommended, as well as special bulk-forming cereals such as wheat bran, linseed or Indian flaxseed. Sauerkraut and soaked dried fruits also have a laxative effect and thus help regulate stool.
Please do not forget: It's very important to drink enough, because the fibre requires adequate liquid in order to properly bulk and be eliminated. In general, you should drink 1.5 to 2 litres of fluid a day. This way the stool becomes very soft and you have to push less.
Last but not least: Please avoid constipating foods like long-steeped black tea, blueberries, grated bananas and apples and - sorry to say - chocolate and cocoa. Also, irritating substances such as coffee and strongly spiced food should be reduced or omitted altogether.
Move, move, move!

As already mentioned, being overweight and lack of exercise are considered risk factors for haemorrhoidal disease. And good intestinal function also requires exercise; after all, humans were not born to sit. Give those hemorrhoids a run for their money, by getting up and getting active.
Whether it is a brisk walk, swimming or cycling, exercise stimulates your digestion, improves blood circulation and thus also the drainage of blood from the haemorrhoidal vessels. Shedding a few unwanted pounds is just another positive side-effect. A true win-win situation!
Please remember: Strength training (e.g. weight lifting), marathon runs or jump-intensive sports (tennis, squash) are counterproductive. The exaggerated movements and stops can put a strain on the pelvic floor and thus also on the vessels in the anal region.
Proper elimination techniques & optimal anal hygiene with ProctyClean®

It is clear that hemorrhoids are caused by excessive pushing during bowel movements, especially when the stool is too hard. In order for the stool to be soft and easier to eliminate, a balanced diet is necessary. The less you push, the less chance you give the hemorrhoids of becoming enlarged!
It is also important that you relax and not rush “number 2”. However, coloproctologists caution against taking too long, and this could lead to involuntary pushing, which increases the pressure on the rectum and worsens the vascular situation there.
A good sitting position is important: it is important to let the buttocks hang properly in order to relieve the blood-filled vascular cushions as much as possible. Even if it sounds funny: A fixed time schedule for going to the bathroom, in order to get the intestine used to a regulated rhythm, is also a successfully proven technique. Suppressing a bowel movement is a no-no, as the stool is only made harder when held back.
After defecation, it is important to thoroughly clean the anal region and the anus. This is best done with lukewarm water. Please do not forget to pat dry with a soft cloth or soft toilet paper and avoid strong rubbing.
Wet wipes are tempting when travelling, but they should be avoided because of the fragrances and preservatives they usually contain. If you still don't want to do without a wet cleaning down under, it is better to use a hand shower or mobile bidet, which are readily available in many drugstores.
With the ProctyClean® intimate hygiene pen, you ensure optimum anal hygiene in the case of haemorrhoidal disorders and prevent the occurrence of secondary diseases caused by leaky stool residue or fluids. ProctyClean® gets to the bottom of the matter: The ProctyClean® intimate hygiene pen, which is moistened with skin-friendly vitamin E oil, is carefully inserted into the anal canal and removes any stool residue with gentle movements. Even residue in the fine skin folds of the anus is removed. Ideally, the entire cleansing process takes place once a day in the shower and lasts only a few minutes. What remains is a clean anal canal, a clean anus and of course a clean anal area for a super clean feeling all day long. Perfect anal hygiene reduces problems!
Hands off laxatives!

No matter how tempting it may be, because bowel movements can be particularly painful in the case of a haemorrhoidal condition, laxatives should not be taken. These should only be used after consultation with the doctor. Prolonged use creates a sluggish bowel and leads to unpleasant constipation. Repeated diarrhoea caused by laxatives also leads to a limited function of the sphincter muscle, and this is guaranteed to get you into trouble!
Use caution when utilizing methods like enemas and anal showers that promise relief. They can damage the intestinal mucosa and flora, as well as the sensitive haemorrhoidal ring – please use only under doctor’s orders. These methods should only be used on occasion and can lead to anal leakage – and you do want to be clean every day, right?
One thing is clear: ProctyClean® eliminates the cause before symptoms occur - and that without unnecessarily irritating the bowel. One daily application that takes just a few minutes is enough. Do you want to feel clean and fresh right away? Click here to process your order.